Virtual and In-person Role Play Simulation on Medication Errors
By: Charlotte Pham, DO, and Jason Chandrapal, MD, Advanced Clinical Simulation Fellows, Durham, North Carolina
A medication error is any preventable event that may cause or lead to inappropriate medication use or patient harm. Such events may be related to prescribing, order communication, product labeling, packaging, nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use. In the United States, 7,000 to 9,000 people die annually due to a medication error, and hundreds of thousands experience adverse reactions or other medical complications. These mistakes also represent a significant financial burden, with the estimated total cost of looking after patients with medication-associated errors exceeding $40 billion each year (Tariq et al., 2021).
In addition to direct patient harm and financial burden, medication errors have a steep psychological cost that can be far wider-reaching. As a facilitator, Jason recounts, "From my personal experience as an intern on a busy surgical service, I forgot to restart a patient's anticoagulation following surgery, and they subsequently developed a blood clot. I felt terrible and disappointed because I felt that the patient trusted me, and I broke that trust. It is a memory that we still vividly remember many years later and fortunately turned it into an opportunity for growth and improvement."
In creating a medication error simulation, we extracted meaningful lessons from analyzing these mistakes in a safe environment. Due to the COVID-19 pandemic, we created a virtual presentation regarding medication errors and introduced a short role-play scenario using selected learners as participants. The scenario focused on a mistaken order for a blood thinner's supratherapeutic dose that led to an intracerebral bleed.
The scenario was followed by a debriefing seeking to identify additional workplace hierarchy, culture, and scope of practice issues that could contribute to future medication errors. We presented this simulation in a virtual setting during the annual SimLEARN Simulation Fellows Education Week and later in-person to the Durham VA Health Care System (DVA HCS) RN Transition to Practice cohort (RNTTP - a comprehensive 12-month program designed to assist the new RN in the transition to full practice as a competent RN). As part of Durham's virtual site visit to achieve SimLEARN's Advanced Tier Level Certification, we presented it to the SimLEARN reviewers to illustrate how a virtual simulation can be useful and engaging.
Virtual learning has increasingly been used during the COVID-19 pandemic. When we delivered our simulation education through two different platforms, we noticed our learners engaged and freely shared their thoughts during both virtual and in-person facilitated discussions. The role-playing allowed learners to practice future roles and better understand the other disciplines' roles and responsibilities.
As one of the facilitators, Charlotte shared her previous personal experiences with pharmacists who caught her mistakes during her residency. In this particular example, where she did not convert pounds to kilograms, there might have been an overdose given to the patient due to this mathematical error. During her internship year, she admitted that she sometimes got annoyed by calls from the pharmacists. However, when recalling these "good catch" experiences, she appreciates pharmacists and their roles.
Our facilitated discussion emphasized the importance of interprofessional collaborative communication and teamwork to promote patient safety. By doing both in-person and virtual simulation education, we were able to reach more learners to deliver our message regarding a patient-centered healthcare approach.
Feedback from the in-person RNTTP session indicated that all participants found that the simulation was worth their time, engaging, and informational. Following the simulation, participants stated they plan to address cultural communication difficulties with coworkers, more confidently advocate for their patients, and reframe their encounters when asking questions to other healthcare professions as a learning or teaching opportunity. In the future we plan to address these intentions to determine the impact of this simulation on behavioral changes.
If any of the VISN Champions would like us to present this simulation during one of their VISN calls, please contact us at charlotte.pham@va.gov or jason.chandrapal@va.gov.
Special thanks to our Durham VA HCS Fellowship Co-Directors, Mary E. Holtschneider and Chan W. Park, and DVA HCS RN Transition to Practice Coordinator, Jody Cherniak, for their collaboration in this educational endeavor.
References Tariq RA, Vashisht R, Sinha A, Scherbak, Y. (2021). Medication Dispensing Errors And Prevention. StatPearls. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK519065/
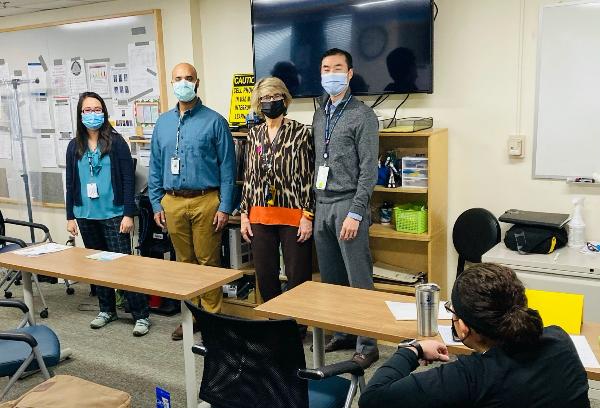
Photo of the authors and the Durham VA SimLearn Codirectors following the in-person medication error simulation to the Durham VA Health Care System RN Transition to Practice learners. (In order from left to right Charlotte Pham, Jason Chandrapal, Mary Holtschneider, and Chan Park. Photo courtesy of Mary Holtschneider)



















