Atlanta team addresses Code 99 in the era of COVID-19
By Joyce Akwe MD, MPH, FACP
Chief of Hospital Medicine
Atlanta VA Health Care System
ATLANTA, Ga. – COVID-19 is the disease that made handshaking a taboo, sheltering in place a way of life, social distancing a must do and face masks, a new fashion trend. This disease demands a change in our way of life and changes in the way we care for patients. COVID-19 is a terrible, fast killing infectious disease. Patients walk into the hospital coughing and can end up dead in a few days. With COVID-19 comes an increase in hospital mortalities and thus the famous, dreaded loudspeaker announcements, "Code 99 room 9c 126, code 99 room 9c 126, code 99 room 9c 126." The heart pounding starts, and the code team realizes that the rules of the game must change in the era of this highly infectious disease.
Code 99 is a medical emergency requiring resuscitation. Creating a protocol for code 99 is not the first thing that comes to mind when we imagine a pandemic like what we are experiencing right now. It did not take a long time to grasp the fact that these are different times and different measures are required. Code teams must make changes to better serve patients who are admitted to the COVID-19 units; the special units created for patients under investigation (PUI) for COVID-19, or patients already diagnosed with COVID-19.
During this era of COVID-19, there have been discussions on the shortage of personal protective equipment (PPE); there has been fast moving and changing information on the most appropriate PPE for the different levels of exposure. Multiple questions on the methods of transmission of COVID-19 and how long the virus can survive on different types of surfaces still linger.
Due to the highly contagious nature of COVID-19, we must make sure that our code team members do not get exposed to the virus. Cross contamination needs to be minimized or eliminated and PPE must be used judiciously, but every code 99 must be managed effectively and efficiently to give our patients the best chance of survival and post cardiac arrest quality of life. To do this, we must make sure that our code teams have the minimum indispensable number of people, and only the crucial equipment is brought into the room.
At the Atlanta VA Health Care System (VAHCS), a COVID-19 code 99 standard of operation was created to address these needs during a code on a PUI for COVID-19 or in patients diagnosed with COVID-19. We identified where the code team members should position themselves inside the room or outside of the room to be able to best perform their responsibilities, and we identified the responsibilities for each code team member. In order to reduce cross contamination, we also clearly identified the objects that could be taken into the room.
An external chest compression device is used in codes for these patients not only to ensure effective and efficient chest compressions, but also to reduce exposure and the number of people that are required to be in the room. With these measures, we reduced the number of people who absolutely needed to be in the room from 13-16 code team members (Akwe, et al., 2019; Prince, et al., 2014) to have on average in most codes to 4 code team members in the room (the code leader, an airway management person, a registered floor nurse and a recorder) for codes in our COVID-19 rooms.
The code cart and the pharmacist or intensive care RN medication nurse stay outside of the room, the nurse floor leader goes in and out of the room, the code assistants and an extra registered nurse stay out of the room in case they are needed in the room.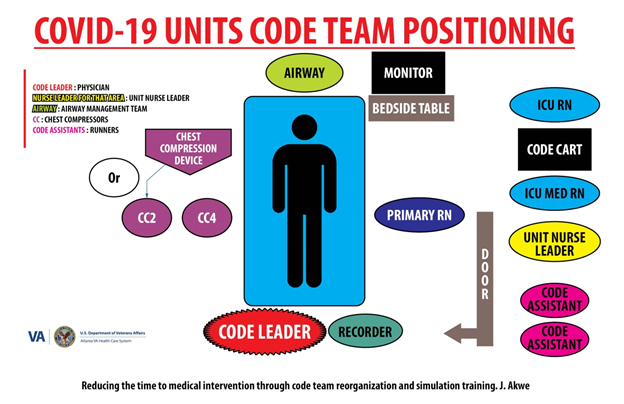
See diagram 1
Every single person involved in the code; be it inside or outside of the room puts on the appropriate PPE.
We hope this model is going to make our codes more efficient with better outcomes, less risk of exposure to the hospital staff and less risk of cross contamination during codes for PUIs or COVID-19 positive patients.
In addition to being chief of hospital medicine, Dr. Akwe is Chair, CPR committee, Atlanta VA Health care System and Associate Professor of Medicine, Emory University School of Medicine.
References
Akwe, J., Gunter, P., Witt, L. S., Cadet, A., Onuorah, E., Fongeh, T., & Huff, L. (2019). Reducing Time to Medical Intervention Through Code Team Reorganization and Simulation Training. Medical Research Archives, 7(12).
Prince, C.R., Hines, E.J., Chyou, P.H., Heegeman, D.J. (2014). Finding the key to a better code: code team restructure to improve performance and outcomes, Journal of Clinical Medical Research, 57, p. 12-47, doi: 10.3121/cmr.2014.1201.
####



















